Non-Invasive Nail Plate Clip Traction for Intra-Articular Thumb Interphalangeal Fracture with Extensor Tendon Injury

Abstract
Intra-articular fractures of the thumb interphalangeal (IP) joint with concurrent extensor tendon laceration present a rare and complex challenge. Conventional methods such as transosseous K-wire fixation or external traction frames may be contraindicated in cases with soft tissue compromise. We report a case in which a novel, non-invasive traction technique using a nail plate clip was employed following surgical tendon repair. Early outcomes demonstrated effective articular alignment and preserved skin integrity. This method may offer a practical alternative to traditional skeletal traction systems in select cases.
Article
Introduction
Fractures involving the thumb IP joint are uncommon, particularly when complicated by soft tissue injury such as extensor tendon laceration. Traditional fixation methods including percutaneous K-wires or external skeletal distractors—carry risks such as pin tract infection, soft tissue irritation, or interference with tendon healing.
While traction methods such as dynamic external fixation have been used effectively in other phalangeal and metacarpal injuries (Schuind et al., 1988), reports of non-invasive traction in the thumb IP joint remain sparse. Here, we describe a modified traction approach using a nail plate clip in the acute postoperative setting.
Case Presentation
A 30-year-old right-hand-dominant male presented to the emergency department with a traumatic injury to the right thumb following an angle grinder accident. Examination revealed a deep laceration over the dorsal IP joint and complete loss of active extension. Radiographs confirmed an intra-articular fracture of the distal phalanx involving the IP joint, with minimal displacement and no subluxation.
Management and Technique
The patient underwent surgical repair of the extensor tendon under appropriate anesthesia. To maintain joint alignment and fracture distraction without the need for skeletal fixation, a non-invasive method was employed:
- A surgical-grade metal clip was adhered to the nail plate using cyanoacrylate adhesive.
- Elastic bands were attached from the clip to a dorsal thermoplastic orthosis, applying continuous longitudinal traction in extension.
- The splint was molded to the forearm and hand, stabilizing the thumb in a neutral to slightly extended position.

Fig.1: Preoperative radiograph showing intra-articular fracture of the distal phalanx at the thumb IP joint.
This construct preserved soft tissue integrity and allowed dynamic adjustment of tension without additional
surgical intervention.
Early Outcome (Day 5)

Fig.2: Day 5 post operative radiograph demonstrating maintained reduction and joint alignment
Five days post-application:
- The patient reported no pain or discomfort.
- The surgical site and nail bed showed no signs of ischemia, ulceration, or adhesive-related damage.
- Radiographs demonstrated maintained alignment of articular fragments and satisfactory reduction.
- No loosening or mechanical failure of the traction system was observed.
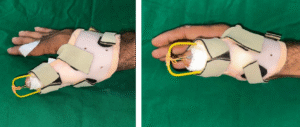
Fig.3: Clinical image of non-invasive nail plate clip traction construct in situ on Day 5
Discussion
The concept of dynamic or static traction using external devices has been successfully applied in metacarpal and phalangeal fractures (Schuind et al., 1988). In that study, a triangular external fixator provided prolonged traction, preserving articular congruity while minimizing soft tissue disturbance. Similarly, the present case employed tension-based alignment without invasive fixation, representing a potential extrapolation of external traction principles into non-invasive thumb IP management.
This method may be particularly useful in acute settings where infection risk, patient comorbidities, or limited resources preclude conventional skeletal traction. Compared to K-wire or mini-external fixator constructs, this approach avoids transcutaneous entry points and may reduce risk of pin site complications and iatrogenic damage to surrounding structures.
Conclusion
This case demonstrates the potential of a non-invasive nail plate clip traction method in managing intra- articular thumb IP fractures complicated by extensor tendon injury. The early radiological and clinical outcomes suggest that this technique may be a viable alternative in select cases, particularly when minimizing soft tissue insult is prioritized. Further evaluation is required to assess long-term joint congruity, tendon healing, and functional recovery.
Consent for publication
Informed written consent for publication and accompanying images was obtained from the patients prior to collecting information.
Availability of data and material
All data generated or analyzed during this study are included in this published article.
Competing interests
The authors declare that they have no competing interests.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- Fufa, D.T., Goldfarb, C.A., Desai, M.J. & Boyer, M.I., 2004. Traction for the treatment of middle phalangeal pilon fractures: a critical analysis. Journal of Hand Surgery, 29(4), pp.785–791. https:// doi.org/10.1016/j.jhsa.2004.03.015
- Sarris, I., Goitz, R.J. & Sotereanos, D.G., 2004. Dynamic traction and minimal internal fixation for thumb and digital pilon fractures. Journal of Hand Surgery, 29(1), pp.39–43. https://doi.org/10.1016/j.jhsa.2003.09.010
- Schuind, F., Noorbergen, M., Andrianne, Y. & Burny, F., 1988. Comminuted fractures of the base of the first metacarpal treated by distraction–external fixation: a new technique. Journal of Orthopaedic Trauma, 2(4), pp.314–321.
- Suzuki, Y., Matsunaga, T., Sato, S. & Yokoi, T., 1994. The pins and rubbers traction system for treatment of comminuted intraarticular fractures and fracture-dislocations in the hand. Journal of Hand Surgery (British and European Volume), 19B(1), pp.98–107.
- Wolfe, S.W., Hotchkiss, R.N., Pederson, W.C., Kozin, S.H. & Cohen, M.S. (eds.), 2017. Green’s Operative Hand Surgery. 7th ed. Philadelphia: Elsevier