Comparative Accuracy and Clinical Utility of Point-of-Care Hemoglobin Analysis Using in Pediatric Craniosynostosis Surgery

Abstract
Background: Craniosynostosis correction in children often results in significant intraoperative blood loss. Accurate monitoring of hemoglobin (Hb) concentration is essential for timely transfusion decisions. Point-of-care (POC) devices such as HemoCue offer rapid hemoglobin estimation but may differ in accuracy compared to laboratory testing.
Objectives: To compare intraoperative hemoglobin levels measured using the POC device with preoperative laboratory values, evaluate the agreement between methods, and assess the reliability of POC in guiding blood transfusions.
Methods: A retrospective analysis was conducted on 40 pediatric craniosynostosis surgeries performed between 2020 and 2024. Preoperative venous blood Hb values from automated laboratory testing were compared with intraoperative capillary samples analyzed using POC. Statistical tests included Shapiro-Wilk, Wilcoxon signed-rank, and Bland-Altman analysis.
Results: The mean difference between lab and POC Hb readings was 0.53 g/dL (SD ±0.65), with a median difference of 0.35 g/dL. While most measurements were within clinically acceptable ranges, some discrepancies reached 2.0 g/dL. Bland-Altman plots confirmed good agreement. Intraoperative transfusions were guided by POC values in 80% of patients, with no reported morbidity.
Conclusion: POC devices provided sufficiently accurate intraoperative hemoglobin readings to guide transfusion decisions during pediatric craniosynostosis surgery. While discrepancies exist, the clinical utility and immediacy of results support its continued use, particularly where lab access is limited
Article
Introduction
Craniosynostosis is a congenital condition characterized by the premature fusion of cranial sutures, leading to abnormal skull growth and elevated intracranial pressure. Early surgical correction is essential to prevent neurodevelopmental delays [1]. However, craniosynostosis surgery is often associated with significant intraoperative blood loss, posing increased risks in young children due to their lower circulating blood volumes [2,3]. Maintaining adequate hemoglobin concentration is critical during these procedures, with transfusion thresholds commonly based on hemoglobin levels falling below 10 g/dL [4]. Although laboratory hemoglobin testing is considered accurate, it is often delayed during surgery. In contrast, POC testing using devices provides rapid bedside hemoglobin estimation; however, concerns remain about its accuracy and the variability of results, particularly with capillary samples [5]. This study aims to assess the clinical reliability of intraoperative POC readings by comparing them with preoperative laboratory values in pediatric craniosynostosis surgeries, evaluating accuracy and variability using Bland-Altman analysis, and determining the impact of POC results on intraoperative transfusion decisions.[3].
Methods
This retrospective observational study included 40 pediatric patients aged 1–10 years who underwent craniosynostosis surgery at the National Hospital of Sri Lanka between 2020 and 2024. Patients were included if they had complete paired hemoglobin measurements from both laboratory testing and intraoperative POC analysis, with no history of preoperative blood transfusion. Those with missing data or complex comorbid conditions were excluded. Preoperative venous blood samples were collected 48 hours prior to surgery, while intraoperative capillary samples—obtained from finger or heel pricks—were taken immediately after the induction of anesthesia and before the administration of significant intravenous fluids or the onset of major blood loss. POC hemoglobin readings were recorded at this point. Statistical analysis was performed using SPSS software. The Shapiro-Wilk test was used to assess the normality of data distribution, while differences between paired hemoglobin values were analyzed using the Wilcoxon signed-rank test. Agreement between methods was evaluated using Bland-Altman plots. Ethical approval for the study was obtained, and retrospective access to patient data was granted by the hospital.
Results
1.Patient Characteristics:
| Variable | Value |
| Total patients | 40 |
| Female | 24 (60%) |
| Male | 16 (40) |
| Age 1-3 years | 82 (70%) |
| Age 3-6 years | 8 (20%) |
| Age 6-10 year | 10 (10%) |
Table 1: Demographic Characteristics of Pediatric Patients Undergoing Craniosynostosis Surgery
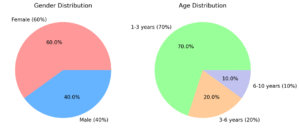
Fig 1: Age and gender distribution of patients who underwent craniosynostosis surgery
2.Comparison of Hemoglobin Readings:
| Parameter | Value |
| Mean difference (Lab – POC) | 0.53 g/dl |
| Median difference | 0.35 g/dl |
| Standard deviation | ±0.65 g/dL |
| Range of difference | 0.1–2.0 g/dL |
| Normality (Shapiro-Wilk test) | p = 0.04 (non-normal) |
| Wilcoxon signed-rank test | p < 0.05 (significant) |
Table 2: Statistical Comparison of Hemoglobin Values Between Laboratory and Point-of-Care Measurements
Discussion
This study confirms that POC provides reliable and timely intraoperative hemoglobin values suitable for clinical decision-making in pediatric craniosynostosis surgeries. Although it showed a minor underestimation compared to laboratory values (mean 0.53 g/dL), this aligns with findings in similar studies [6–9]. The significance of the Hb difference (Wilcoxon test, p < 0.05) indicates consistent variability, but most discrepancies remained clinically acceptable. The Bland-Altman plot demonstrated agreement within ±1.96 SD in 95% of cases, reinforcing previous research supporting POS’s utility in surgical and ICU settings [7,8].
Limitations include the retrospective design, absence of venous POC samples for comparison, and potential dilution effects due to fluid shifts during surgery. Despite these, transfusions based on POC values resulted in favorable clinical outcomes, with no reported morbidity.
Conclusion
POC devices offer practical and reasonably accurate intraoperative hemoglobin monitoring in pediatric craniosynostosis surgery. While minor discrepancies exist, they are not clinically significant in most cases. The device facilitated timely transfusion decisions and ensured safe surgical outcomes.
Limitations
-Retrospective design.
-No concurrent venous sampling.
-Possible fluid-related dilution not fully quantified.
Recommendations
-Conduct prospective studies using simultaneous capillary and venous sampling. Employ serial Hb measurements to observe trends post-transfusion.
-Evaluate POC device accuracy across broader pediatric surgical populations.
Conflict of Interest
No conflict of interest declared. The HemoCue device was used without external sponsorship or manufacturer involvement.
Declarations
None
Consent for publication
Informed written consent for publication and accompanying images was obtained from the patients prior to collecting information.
Availability of data and material
All data generated or analyzed during this study are included in this published article.
Competing interests
The authors declare that they have no competing
interests.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- Pearson, A. and Matava, C.T., 2016. Anaesthetic management for craniosynostosis repair in children. BJA Education, 16(12), pp.410–416. https://doi.org/10.1093/bjaed/mkw023.
- Goodrich, J.T., n.d. Cranioplasty Techniques. In: I8, [online] Neupsykey.com. Available at: https:// neupsykey.com/cranioplasty-techniques/ [Accessed 9 Jul. 2025]
- Park, C., Wormald, J., Miranda, B.H., Ong, J., Hare, A. and Eccles, S., 2018. Perioperative blood loss and transfusion in craniosynostosis surgery. Journal of Craniofacial Surgery, 29(1), pp.112–115. https://doi.org/10.1097/SCS.0000000000004098.
- Royal Children’s Hospital Melbourne. (n.d.). Blood product prescription. https://www.rch.org.au/clinicalguide/guideline_index/Blood_product_prescription/
- Brehm, R., South, A. and George, E.C., 2024. Use of point-of-care haemoglobin tests to diagnose childhood anaemia in low- and middle-income countries: A systematic review. Tropical Medicine & International Health, 29(2), pp.73–87. https://doi.org/10.1111 tmi.13957.
- Kim, S.-H., Lilot, M., Murphy, L.S.-L., Sidhu, K.S., Yu, Z., Rinehart, J. and Cannesson, M., 2014. Accuracy of continuous noninvasive hemoglobin monitoring: A systematic review and meta-analysis. Anesthesia & Analgesia, 119(2), pp.332–346. https://doi.org/10.1213/ANE.0000000000000272.
- Sanchis-Gomar, F., Cortell-Ballester, J., Pareja-Galeano, H., Banfi, G. and Lippi, G., 2012. Hemoglobin point-of-care testing: The HemoCue system. Journal of Laboratory Automation, 18(3), pp.198–205. https://doi.org/10.1177/2211068212457560.
- Patel, A.J., Wesley, R., Leitman, S.F. and Bryant, B.J., 2013. Capillary versus venous haemoglobin determination in the assessment of healthy blood donors. Vox Sanguinis, 104(4), pp.317–323. https://doi.org/10.1111/vox.12006.
- Spilka, J. and Goobie, S.M., 2020. Perioperative blood management in the pediatric patient. Edited by F. Evans. Boston Children’s Hospital. Published 18 February 2020. Available at:Jared. [email protected] [Accessed 9 July 2025].