Successful Staged Macrocephaly Reduction Surgery in SriLanka

Abstract
Background: Severe macrocephaly from untreated infantile hydrocephalus is rare but still encountered in low-resource settings. Without timely diversion, progressive calvarial expansion and developmental delay can ensue.
Case: A boy with antenatally diagnosed hydrocephalus had parental refusal of shunting in infancy and was lost to follow-up. He presented at 7 years with extreme macrocephaly and profound gross motor delay but relatively preserved speech and cognition. A staged strategy (initial ventriculo-peritoneal [VP] shunt, dural release, serial anterior/posterior cranial vault reductions, and final contouring) was performed across two years. Complications included a prolonged cerebrospinal fluid (CSF) leak that settled conservatively and formation of a “dual skull” (intradural neobone with extradural hydroma) requiring further reduction. By the end of staged surgery and intensive physiotherapy, he achieved independent ambulation with minimal support and a near-normal head position.
Conclusion: In older children with long-standing hydrocephalic macrocephaly, staged reduction cranioplasty following CSF diversion can restore function and cosmesis when paired with structured rehabilitation. Early shunting remains standard of care, but delayed staged reduction is a viable salvage pathway.
Article
Introduction
Macrocephaly is a head circumference >2 SD above the age-matched mean. When due to untreated hydrocephalus, the head can become too large and heavy for postural control, impairing gross motor development and quality of life. While VP shunting or endoscopic third ventriculostomy (ETV) are the guideline-supported mainstays of infant hydrocephalus, late presenters may need calvarial volume reduction to regain head control and mobility.
Case Description
Master L, the second-born child of non-consanguineous parents, was delivered at 32 weeks of gestation by elective caesarean section after antenatal ultrasound revealed congenital hydrocephalus. Despite counseling, his parents declined ventriculoperitoneal (VP) shunting in infancy due to concerns regarding anesthesia and surgery, and defaulted subsequent follow-up. At seven years of age, he presented to the neurosurgical unit with massive macrocephaly, profound gross motor delay, absence of head control, and reliance on “floor-dragging” mobility. Interestingly, cognitive function, language, and comprehension were relatively preserved, and there was no history of seizures or raised intracranial pressure symptoms.
Figure 1: Master L prior to the treatment of macrocephaly in 2016
Procedures
The management goal was to reduce cranial volume, restore head balance, and facilitate developmental progress in a child with otherwise preserved intellectual ability. A staged surgical approach was undertaken.
Stage 1 – CSF Diversion and Dural Release
A medium-pressure VP shunt was placed for cerebrospinal fluid (CSF) diversion. Postoperative imaging demonstrated a chronic subdural hematoma, necessitating shunt ligation and decompression. Subsequently, a craniectomy with meticulous release of dural adhesions along the superior sagittal sinus was performed. The postoperative period was complicated by a prolonged CSF leak, which eventually resolved without re-operation.

Figure 2: CT scan of brain (axial view) obtained in 2022 October, after 1st anterior vault reduction and reconstruction, yet showing significant compression of brain matter
Stage 2 – Anterior Vault Reduction and Reconstruction
An anterior cranial vault reduction was performed with mesh plate reconstruction, which significantly improved frontal bossing and cranial balance. Following this intervention, the child achieved partial head control and demonstrated improved speech, making him a candidate for further reconstructive stages.
Stage 3 – Posterior Vault Reduction.
A posterior vault reduction was performed through a coronal parieto-occipital approach with mesh fixation. Follow-up imaging revealed dual calvaria formation, with new ossified bone developing along the dura and a fluid plane separating it from the outer cranial vault.
Stage 4 – Final Vault Reduction and Contouring
Residual cranial deformities and excess ossified bone were excised, and contour harmonization was achieved using mesh reconstruction.
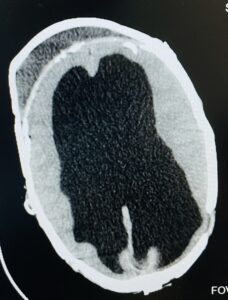
Figure 3: CT scan of brain (axial view) obtained in 2023 May, after shunt removal and awaiting further surgery
Outcome
The child underwent intensive physiotherapy focusing on cervical and paraspinal extensor strengthening, gait training, and postural control. By four years after initial presentation, he was able to maintain near-normal head positioning, walk independently with minimal support, and achieve a satisfactory cosmetic outcome.

Figure 4: Photos of Master L taken in August 2024, who is now able to walk with support and converse well

Figure 5: Photos of Master L taken in August 2024, who is now able to walk with support
Discussion
Contemporary evidence-based guidance (Congress of Neurological Surgeons, original 2014 and 2020 update) supports CSF diversion with VP shunt or ETV depending on etiology, age, and anatomy. ETV (often with choroid plexus cauterization in infants) has expanded but shunting remains predominant in infants; large networks (e.g., HCRN) have protocolized shunt care and infection mitigation. Ongoing trials continue to compare ETV/CPC with shunting in early infancy. Implication for late presenters: For children who miss early diversion and develop hydrocephalic macrocephaly, shunt alone rarely reduces head circumference sufficiently for postural recovery; reduction cranioplasty becomes a reconstructive adjunct.
A 2024 systematic review of 27 studies reported improvements in head positioning, cosmesis, and global function after reduction cranioplasty, with notable blood loss and shunt-related complications underscoring the need for careful selection and experienced teams. Long-standing ventriculomegaly “pushes” the calvaria outward while sutures typically remain patent/diastatic. After shunt placement, a distinct entity shunt-related (secondary) craniosynostosis can occur, likely from loss of dural/sutural tension, with premature fusion of one or more sutures and thickened vault; reported but variable in incidence, it complicates head shape and may require remodeling.
Large, single-session reductions risk venous kinking and infarction (given inability to “shorten” superior sagittal sinus and skull base) and abrupt brain infolding. Staging allows gradual extracranial volume normalization while respecting venous outflow. Technique families (e.g Mechanism: how the VP shunt “sets the stage” for head-size reduction. VP shunting lowers intraventricular pressure and reduces ventricular volume, enabling the brain to re-expand (in infants) or, in long-standing cases, to “settle” within the capacious skull but the osseous envelope usually remains oversized. Diversion also predisposes to subdural collections during rapid pressure shifts, a known shunt effect that often requires management before definitive vault work.
In hydrocephalic macrocephaly, the dura can be tethered to the ectatic inner table, especially near the superior sagittal sinus. Extradural (endocranial) release; careful subperiosteal/epidural dissection and lysis of dural adhesions; restores dural mobility and makes subsequent segmental reductions safer by minimizing venous traction. This step, used in our case prior to vault reduction, helped the brain “settle” gradually before external volume reduction.
Operative strategies then combine partial-thickness osteotomies, segmentation (quadrants/“picket fence”), controlled wedge resections, and mesh-assisted refashioning; programmable valves can be considered where suture fusion or over-drainage complicate shape.
The dura mater is osteogenic; it orchestrates calvarial morphogenesis by secreting growth factors and recruiting osteoprogenitors. After dural release/reconstruction, intramembranous ossification over the dura can create an inner neocalvaria, clinically visualized as a “dual skull” with a fluid plane (hydroma) between inner and outer tables, as in our patient. This phenomenon is well documented experimentally and clinically.
Years of macrocephaly lead to cervical extensor hypoplasia and poor trunk control. Pediatric neuro-physiotherapy focusing on cervical extensor strengthening, postural control, vestibular/righting reactions, and progressive gait training is essential; recent pediatric case reports in hydrocephalus show meaningful gains in head/trunk control and gross motor milestones with structured programs. Aquatic or ball-based interventions can augment cervical activation when tolerated.
Conclusion
This case highlights that, even after late presentation, a staged pathway CSF diversion, dural/endocranial release, serial volume reductions and contouring can yield functional independence and acceptable aesthetics when paired with targeted rehabilitation. Early shunting remains the standard; however, delayed, staged reduction is a valid salvage strategy in carefully selected older children.
Acknowledgements
We acknowledge the multidisciplinary Neurosurgery, Plastic Surgery, and Physiotherapy teams involved in the child’s care.
ORCID
Gayan Ekanayake https://orcid.org/0000-0001-8420-7073
Shathir Ahamed https://orcid.org/0009-0008-0716-4143
Consent for publication
Informed written consent for publication and accompanying images was obtained from the patients prior to collecting information.
Availability of data and material
All data generated or analyzed during this study are included in this published article.
Competing interests
The authors declare that they have no competing interests.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- Moura SP, Center AD, Kalluri M, Blum J, Shaffrey EC, Lee S, Ng JJ, Iskandar BJ, Garland CB, Cho DY. Reduction cranioplasty for hydrocephalic macrocephaly: a systematic review of surgical outcomes. J Neurosurg Pediatr. 2024 Jun 21:1-13. doi: 10.3171/2024.4.PEDS23486. Epub ahead of print. PMID: 38905711.
- Gage EA, Price AV, Swift DM, Sacco DJ, Fearon JA. Limited reduction cranioplasty for the treatment of hydrocephalic macrocephaly. Plast Reconstr Surg. 2011 Dec;128(6):1272-1280. doi: 10.1097/PRS.0b013e3182221404. PMID: 22094746.
- Choi, JI., Dhong, E.S., Lim, DJ. et al. Reduction cranioplasty for macrocephaly with long-standing hydrocephalus and non-fused fontanelle in Chiari malformation type I. Childs Nerv Syst 30, 1763–1766 (2014). https://doi.org/10.1007/s00381-014-2451-2
- Moura, Steven P et al. “Reduction cranioplasty for hydrocephalic macrocephaly: a systematic review of surgical outcomes.” Journal of neurosurgery. Pediatrics (2024): 1-13.
- Suryaningtyas, Wihasto & Parenrengi, Muhammad. (2020). Case Report: Cranial Vault Reduction Cranioplasty for Severe Hydrocephalus. Folia Medica Indonesiana. 56. 154. 10.20473/fmi.v56i2.21237.
- Moura, S.P., Alencar, E.P., Carvalhal, M.C., Saleme, S. and Ferreira, N.P., 2024. Reduction cranioplasty for hydrocephalic macrocephaly: A systematic review of surgical outcomes. Journal of Neurosurgery: Pediatrics, 34(2), pp.136–143. https://doi.org/10.3171/2024.4.PEDS23486
- Bauer, D.F., Baird, L.C., Klimo, P., Mazzola, C.A., Nikas, D.C., Tamber, M.S. & Flannery, A.M., 2020. Congress of Neurological Surgeons systematic review and evidence-based guidelines on the treatment of pediatric hydrocephalus: update of the 2014 guidelines. Neurosurgery, 87(6), pp.1071-1075. https://doi.org/10.1093/neuros/nyaa434
- Mathews, M.S., Loudon, W.G., Muhonen, M.G. & Sundine, M.J., 2007. Vault reduction cranioplasty for extreme hydrocephalic macrocephaly. Journal of Neurosurgery: Pediatrics, 107, pp.332-337. https://doi.org/10.3171/PED-07/10/332