Post Operative Monitoring In Microsurgery: Comparing Glucose Measurement With Clinical Parameters.

Abstract
Traditionally clinical monitoring of microvascular surgery in the postoperative period requires a clinician to monitor the flap by various clinical parameters. The objective of this study was to evaluate post operative blood glucose monitoring within flap and compare it with traditional clinical parameters and use as a tool that can help in early detection of flap complication. We performed 38 free flaps, 7 critical revascularisation and 9 replantations. Blood glucose was checked at the normal finger tip of the patient and simultaneously flap was scratched or replanted limb or digits were pricked and blood sugar noted. Blood glucose monitoring was performed at regular interval. There were 20 complications out of which 7 underwent minor intervention and 13 underwent major intervention. Eleven interventions resulted in normalisation of tissue perfusion, with a salvage rate of 55%. Glucose levels were significantly correlated to other clinical parameters. Sugar levels were significantly low in the complication group, either its absolute level or its difference to normal digit glucose level. We conclude that the measurement of free tissue capillary glucose level may be used as method of diagnosis of complication, but it is not superior to clinical evaluation by an experienced professional.
Article
INTRODUCTION
Free-tissue transfer and replantation or revascularization are accepted part of the armamentarium of reconstructive surgeons with quoted success rates around 95% [1]. The success of these surgeries is dependent on the continuous arterial inflow and venous outflow through patent microvascular anastomoses until neovascularization is established by peripheral ingrowth of capillaries. Traditionally, monitoring of free flaps and replantations in the postoperative period requires a clinician to monitor the flap or replanted parts by various parameters [2]. Blood glucose measurement from flap or replanted tissues establishes a simple method that can be used widely to decrease the flap loss rate after free tissue transfers and replantations [3].
METHODS
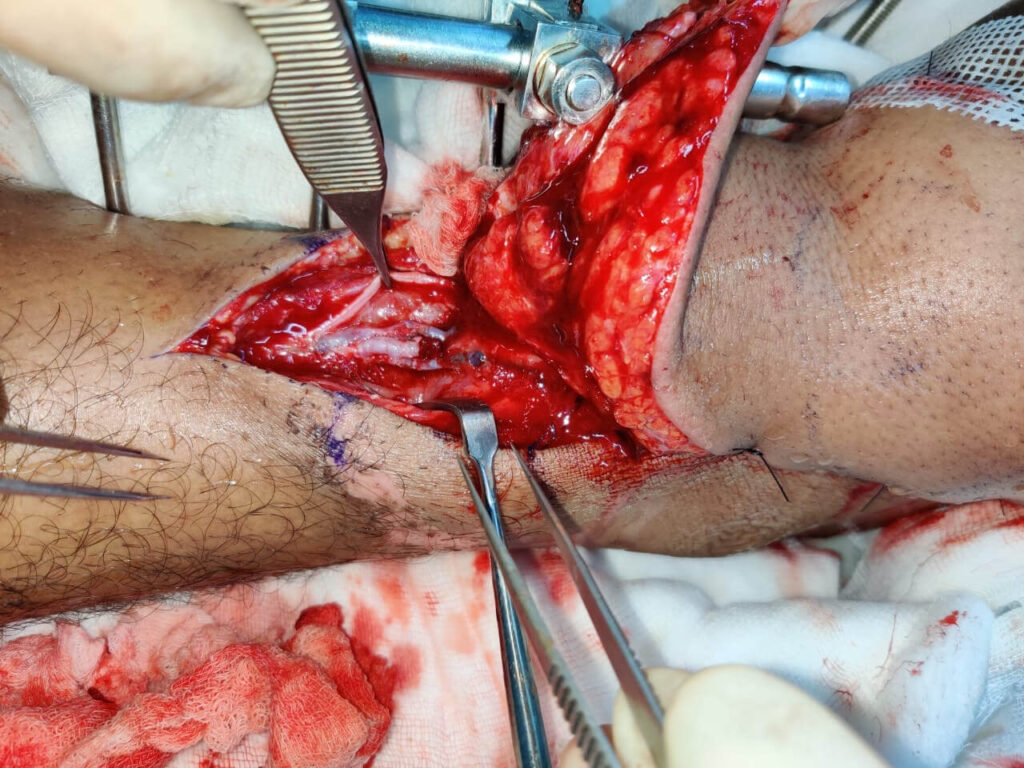
This study was conducted at the department of Plastic Surgery at a tertiary care hospital, which is also a resident training institute in India. It was done from January 2021 to June 2022 over a period of 18 months. All the patient undergoing microvascular surgery, either free tissue transfer or replantation or revascularizations were included in the study. Patients with history of diabetes, history of chronic steroids intake and patients not consenting for the study were excluded.
Any patient who underwent surgery which resulted in a considerable defect e.g. surgery for malignancy, which required reconstruction by free tissue transfer which needed the microvascular anastomosis or the patients with amputation of any part of limb or organ which came under indication for replantation or revascularization were recruited in the study after taking due consent. We had three groups of patients in this study:
- Free tissue transfer
-
Critical revascularization
-
Replantation
The patients were admitted and worked up for the surgery. All history, clinical examination and investigations were done accordingly. All patients underwent at least one arterial and one venous anastomosis as was required for every microsurgical free flap or replant operation.
In the post operative patient were observed for vitals, urine output, flap perfusion clinically, hourly for the first twelve hours and then twice daily over the next five days. The patient was observed initially in post-op recovery for initial 1-2 hours till he/she was fully stable hemodynamically. Then the patient was shifted to high dependency unit (HDU) for further monitoring. The replanted part/ free transferred tissue were monitored at regular interval with all parameters described below.
The sugar level was measured by needle prick with 26G needle is done in flap and finger. Glucose level is measured with Free Style Optium Neo instant instruments which utilize very small quantity of blood (≈10 μl).
In case of deranged value/clinical situation which were indicated to intervene early, the patient was shifted to the operation theatre immediately for the intervention. In this situation the intervention performed was noted and the tissue was monitored further. These patients were followed up serially, initially hourly and then twice a day.
RBS Monitoring
| 1 Hour | 2 Hours | 3 Hours | 6 Hours | 12 Hours | 24 Hours | 48 Hours | 72 Hours | |
| Replanted part/Flap | 110 | 118 | 136 | 122 | 132 | 126 | 122 | 111 |
| Normal limb | 215 | 166 | 182 | 175 | 160 | 153 | 139 | 107 |
| Clinical parameters | ||||||||
| Colour of flap | Normal | Normal | Normal | Normal | Normal | Normal | Normal | Normal |
| Turgor of flap | Good | Good | Good | Good | Good | Good | Good | Good |
| Temperature | Warm | Warm | Warm | Warm | Warm | Warm | Warm | Warm |
| Capillary refill time | <3 sec | <3 sec | <3 sec | <3 sec | <3 sec | <3 sec | <3 sec | <3 sec |
| Colour of blood on scratch/pin prick | Bright red | Bright red | Bright red | Bright red | Bright red | Bright red | Bright red | Bright red |
RESULTS
A total of 54 patients were included in the study. Among the groups, Group 1 included 38 patients (25 men and 13 females) ranging from 10 to 74 years (Mean-37.84), Group 2 had 7 patients ranging from 10 to 52 years (Mean-27), and Group 3 had 9 patients ranging from 10 to 52 years (Mean- 33.44).
Out of 54 patients, 34(63%) patient did not require any intervention and the tissue survived without any complications. A total of complications occurred in 20 patients overall including all the groups.
The complications which occurred in the form of congestion or occlusion or hematoma was 11 in Group 1(28%) out of which venous was more common i.e., 9(81% of total complications) and arterial 2(19%). In group 2, there were 3 complications (42%) out of which 2 were venous and 1 was arterial, and in group 3 there were 6(66%) complications out of which 4 were venous and 2 were arterial. Venous complication occurred later (Mean 19.4 hrs) than arterial (Mean 2.8 hrs). All flap complication patients underwent intervention either minor in the form of rewarming, Leech therapy, clot removal or major in the form of re-exploration and revision of anastomoses. Out of total 20 complications 7(35%) underwent minor intervention and 13 (65%) underwent major intervention. The overall salvaged flap after intervention was 11(55%). Where in Free flaps it was 7 out of 11(63%); In revascularization group it was 2 out of 3(66%); and in Replantation group it was 2 out of 6 complications (33%).
The process of salvage was started on clinical basis at once there were sign of complication on clinical grounds. The sugar level difference was significant in those cases at the time of decision making. In two of the cases where clinical parameters were borderline the sugar level difference helped us to decide for intervention.
Table: Comparison of RBS in flap site between Complication group and No complication group
|
RBS(mg/dl) at Flap site |
Complication group(n=20) {median(IQR)} |
No complication group(n=34) {median(IQR)} |
P value (Mann Whitney U test |
P value of difference |
|---|---|---|---|---|
|
At 1 hour |
90.00(74.74 to 119.75 |
96.50(73.00 to 122.25) |
0.507 |
0.485 |
|
At 2 hour |
95.50(71.50 to 135.00) |
114.50(89.50 to 136.50) |
0.107 |
0.014 |
|
At 3 hour |
81.00(46.75 to 124.25) |
114.5(101.25 to 144.25) |
0.005 |
0.007 |
|
At 6 hour |
68.00(30.00 to 107.00) |
107.0(91.75 to 135.0) |
0.006 |
0.051 |
|
At 12 hour |
68.00(0.00 to 126.00) |
108.00(94.00 to 132.25) |
0.027 |
0.001 |
|
At 24 hour |
62.00(0.00 to 109.00) |
107.50(87.0 to 124.50) |
0.001 |
0.004 |
|
At 48 hour |
52.50(0.00 to 123.00) |
108.50(93.25 to 133.25) |
0.004 |
0.000 |
|
At 72 hour |
0.00(0.00 to 68.00) |
106.00(97.75 to 124.00) |
0.000 |
0.000 |
DISCUSSION
The salvage of congested flap depends upon early detection of congestion and timely intervention / re-exploration. The decision to inform the patient for a repeat surgery remains critical, and needs to be backed by objective data.
For monitoring microvascular free tissue transfers, a variety of methods have been described, including a physical assessment of the flap (colour, capillary refill time, temperature and turgor), laser Doppler flowmetry, hand-held acoustic Doppler, non-invasive ultrasound Doppler, implantable micro Doppler system, near infra-red spectroscopy and microdialysis.
In the present study, we compared the blood sugar level of the flap to other commonly used parameters. We analysed whether the falling sugar level as compared to normal finger correlates with the complication occurring in the flap. The study showed that falling blood glucose level strongly correlates with other traditional parameters which can early detect the failing flap or replant to intervene so that to prevent it to enter into non-salvageable stage.
In the present study, we included all microvascular surgery including free flaps and replantation and critical revascularisation, whereas other studies like Deviprasad et al studied only on free flaps. Bashir et al studied free flaps as well as pedicled flaps. A case report by Kazufumi et al describes successful lip replantation with was monitored with blood glucose level and intervention with leech therapy once low sugar level (<40 mg/dl) was detected and flap was salvaged[7].
In the present study, we monitored blood sugar level at 1,2,3,6,12,24,48 and 72 hrs, whereas in other studies (Deviprasad et al and Bashir et al), the evaluation was performed at 0,6,12,24 and 48 hrs[5,6].
The present study analysed blood glucose level from fingertip and not the venous blood glucose level and compared with that of flap and the ratio is calculated for better results. The glucose level along with other parameters was also taken for flap monitoring. The differences in glucose level of flap/replanted part and normal fingertip was compared accordingly.
According to Hara et al. (2011), who reported the test for flap monitoring in 2011, the cutoff value for diagnosing venous bleeding is a blood glucose level of 62 mg/dl in the flap[4]. But this alone reading does not give proper information for re exploration. In some cases, surgeons have found that flaps with a blood glucose level of 62 mg/dl survived, whereas in other cases, flaps necrosed.
The sugar level of flap or replanted part drops in case there are vascular complications. More reliable is the continuous falling sugar level and the difference in sugar level as compared to normal finger sugar level. However, these parameters solely should not be considered as criteria for early intervention. The falling sugar level and very low level as compared to normal level should be additional criteria along with other traditional clinical parameters. In other previous studies like Hera et al, Bashir et al and Chaudhary et al, pedicled and free flaps were studied altogether whereas in the present study we included only free tissue transfer and replantation which was done through microvascular anastomosis. We sought to specifically assess the trend of flap glucose level where microvascular anastomosis was performed.
Advantages
-
Complication in the veins can be detected at an early stage when blood glucose levels fall below the normal range in compromised flaps.
-
The blood glucose level within the flap monitoring method reported in the research is simple and may be carried out by residents, nursing staff, or even patients’ attendants.
-
This is a very cost-effective solution.
-
Tissue transfers using a tiny skin paddle or intraoral flaps, when other typical procedures make monitoring glucose levels impossible, might benefit from using the flap’s blood glucose level as a marker.
Disadvantages
-
The use of this procedure is restricted in situations when vascular integrity has been compromised since in such situations, sufficient blood may not be collected or there may not be any flow at all to assess the glucose level in a pinprick test.
-
Moreover, since blood glucose levels in diabetes patients often fluctuate at both higher and lower values more than they do in non-diabetics, it is uncertain if blood glucose levels obtained from diabetic patients can be used for flap monitoring. Therefore, it could be necessary to modify the blood glucose readings received from diabetes individuals, and further study is needed on this subject.
-
This approach is not suitable for buried tissue transplantation or exclusively muscle flap instances.
-
To yet, this method has not been able to define a cut-off value, sensitivity, or specificity for the diagnosis of early flap congestion
-
The glucometer devices have error of +/- 15% to venous blood glucose level so the value can be erroneous.
-
Blood which is taken from the flap or replanted part may be mixed with tissue fluid or saliva in case of flap in oral cavity.
Further possibilities
This study included free flaps as well as critical revascularizations and replantation of limb or digits as well. Larger sample size in each group would substantiate the results. Other biochemical parameters like lactate level can also be included in post operative monitoring criteria to bring out the easier methods for early detection of failing flaps or replantation.
CONCLUSION
Flap capillary glucose monitoring is an easy, accessible and cost-effective method, which helps in early detection of flap congestion, even before flap discoloration occurs. A falling blood glucose level after microvascular anatomosis strongly correlates with other clinical parameters. The incorporation of blood glucose measurement in addition to clinical monitoring, aids in early detection and possible reduction of post-operative complications due to venous thrombosis.
References
-
Schusterman MA, Miller MJ, Reece GP, Kroll SS, Marchi M, Goepfert H. A single center’s experience with 308 free flaps for repair of head and neck cancer defects. Plast Reconstr Surg 1994;93:472–8.
-
Malt RA, McKhann CF. Replantation of severed arms. JAMA. 1964;189(10):716–22.
-
Kleinert HE, Kasdan ML, Romero JL. Small blood-vessel anastomosis for salvage of severely injured upper extremity. J Bone Joint Surg Am. 1963;45(4):788–96.
-
Tachi K, Mori M, Tsukuura R, Hirai R. Successful microsurgical lip replantation: Monitoring venous congestion by blood glucose measurements in the replanted lip. JPRAS Open. 2017 Dec 12;15:51-55. doi: 10.1016/j.jpra.2017.11.002.
-
Tazeen A, Sulli D. (2020). Evaluation of post-operative blood glucose monitoring as a objective tool for flap monitoring. International Journal of Surgery Science. 4. 145-148. 10.33545/surgery.2020.v4.i1c.325.
-
Bashir MM, Afzal S. Diagnostic Accuracy of Blood Glucose Measurements in Detecting Venous Compromise in Flaps J Craniofac Surg 2015;26: 1492-4.
-
Hara H, Mihara M, Iida T, Narushima M, Todokoro T, Yamamoto T, Koshima I. Blood glucose measurement for flap monitoring to salvage flaps from venous thrombosis. J Plast Reconstr Aesthet Surg. 2012 May;65(5):616-9.
-
Singhal S, Singhal V. “Measurement of blood glucose level ratio for microvascular flap monitoring.” International journal of medical and biomedical studies (2019): n. Pag.
-
Choudhary AK, Singh AI, Das SI, Singh LO, Singh NS. Role of flap blood glucose measurement in monitoring of flap incorporating skin and to detect flap congestion and flap salvage. J Med Soc 2020;34:106-10.

