Large epidermal cyst in the ischiorectal fossa: A rare cause for a perineal lump

Article
Introduction
Epidermal cysts are a rare cause of ischiorectal fossa lesions and only a few cases are reported in the literature. They can grow asymptomatically into significant sizes before becoming externally apparent. History of trauma and previous surgery in the perineum including episiotomy could be recognized as aetiological factors. We report a case of a large epidermal cyst in the right ischiorectal fossa in a 68-year-old female.
Case Presentation
A 68-year-old female patient presented with an insidious onset, gradually increasing, painless swelling in the right perineal and buttock region for six months duration. She denied any symptoms of bowel or anal pathology. There was no history of any perianal trauma or previous surgery except for an episiotomy on the right side at her first child delivery at the age of 33 years. Her medical history was unremarkable. Clinical examination revealed a non-tender, well-demarcated, firm, slightly lobulated, subcutaneous lump in the right perianal region. Vaginal and digital rectal examinations revealed a palpable lump abutting on their walls from the right side. MRI revealed a well-circumscribed unilocular thin-rimmed 10.2×7.7x5x4 cm-sized cystic lesion in the right ischiorectal fossa suggestive of an epidermal cyst (Figure 1). The rectum and the vagina were contralaterally displaced. The patient was operated under general anaesthesia in the prone position with a pillow under the groin area to closely resemble prone-jack knife position. A curved incision was made keeping the convexity away from the anus and the cyst was dissected off around its well-demarcated plane of dissection. Medially it was abutting on the external anal sphincter, which was identified and carefully preserved. The wound was closed in layers over a suction drain and the skin was sutured with intradermal sutures (Figure 2). An occlusive dressing was applied to prevent post-operative faecal contamination. The patient had an uneventful recovery and the histology of the specimen revealed an epidermal cyst measuring 12x8x6 cm without evidence of malignancy. Follow-up after one year was unremarkable without evidence of recurrence or any scar complication.
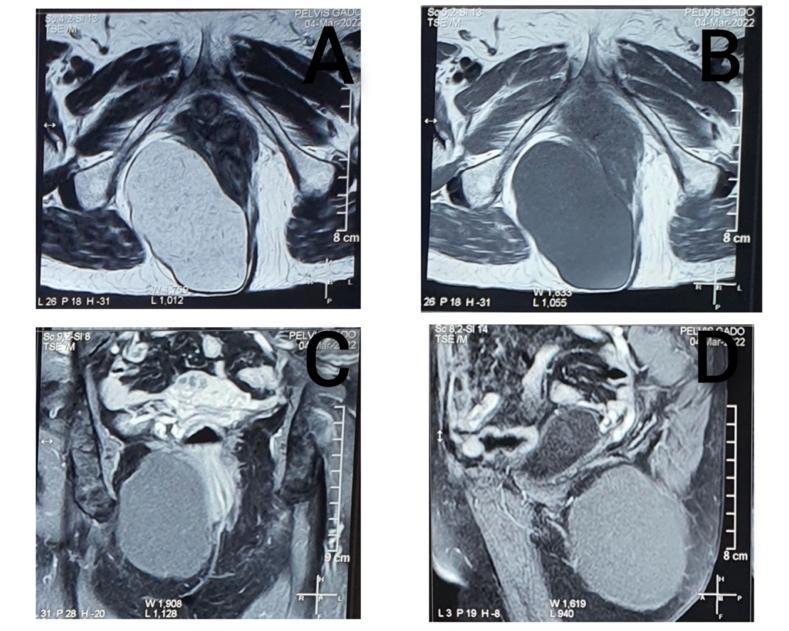
Figure 1: Selected cuts from the MRI
A – T2 axial image showing hyperintense cyst displacing the vagina and the rectum
contralaterally
B, C, D – T1 images showing hypointense cyst with a rim having low signal intensity
signal (B- Axial pre-contrast, C- coronal post-contrast fat-saturated, D – sagittal
post-contrast fat-saturated)

Figure 2: Clinical images
A- Externally visible lump
B. The patient was positioned in the prone position and the incision marked
C- Cyst excised
D- Layered closure with intradermal sutures to skin over a suction drain
Discussion and Conclusions
Epidermal cysts are squamous epithelium-lined keratin-filled cystic lesions. They can be either congenital (from ectodermal remnant) or acquired secondary to trauma (accidental or following a surgical procedure) or due to sebaceous duct obstruction. They commonly occur in the face, neck, extremities and scalp.
Epidermal cysts in ischiorectal fossa are uncommon with only a few case reports published in literature. The common differential diagnoses for lesions in the ischiorectal fossa include abscesses, lipoma, neurofibroma, tailgut cysts, rectal duplication cysts, Gartner duct cysts, Bartholin cysts and rarely carcinomas such as extramucosal anal adenocarcinomas [1].
Epidermal cysts in the ischiorectal fossa are mostly present as slowly enlarging asymptomatic swellings. They can grow into larger sizes usually displacing the adjacent structures; the anus and the vagina in females and may extend to the pelvic space [2]. The largest reported epidermal cyst in the ischiorectal fossa measured 15×10 cm and the largest reported epidermal cyst anywhere measured 17.8×13.18 cm and the latter was located in the gluteal region [3][4].
Theoretically, the possible etiological factor for the cyst in this location in our patient is the previous episiotomy. However, it is important to note that it has taken a long time (35 years) for the appearance of the lump.
MRI is the preferred method of imaging to differentiate from other lesions and to delineate the soft tissue anatomy. They appear as unilocular cysts and the contents are hyperintense on T2-weighted images. T1 weighted mages will show low to high signal intensity, depending on the relative amount of sebaceous or protinaceous material. Their thin wall could enhance with contrast (Figure 1). Malignancy needs to be ruled out in the presence of septa, thick enhancing rim or post-contrast images showing indistinct enhancement of adjacent soft tissues. Although a CT scan can localize the lesion in the ischiorectal fossa, differentiation and characterization are almost impossible and non-specific [1].
Other than the large cyst having the possibility of giving rise to symptoms due to displacing and narrowing down of adjacent structures they can be complicated either by rupture or infection. There is a potential risk for malignant transformation [5].
Surgical excision is the management of choice. Planning of the incision and meticulous dissection to prevent any rupture and spillage of the contents and especially to avoid inadvertent damage to the external anal sphincter, are essential. Care should be taken to avoid faecal contamination to prevent wound infection during the postoperative period. In this case, we utilized a nonlinear skin incision keeping its convexity away from the anal orifice to prevent any damage to the external anal sphincter and for the convenience of managing the post-operative period avoiding faecal contamination of the wound.
Learning points
-
Epidermal cysts are a rare cause of lesions in the ischiorectal fossa and they can asymptomatically grow into large sizes until they are externally apparent.
-
Planning of the incision and meticulous dissection avoiding inadvertent injury to adjacent structures are essential to avoid surgical complications.
Declarations
None
Ethics approval and consent to participate
Not applicable
Consent for publication
Informed written consent for publication and accompanying images was obtained from the patients prior to collecting information.
Availability of data and material
All data generated or analyzed during this study are included in this published article
Competing interests
The authors declare that they have no competing interests.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- Sergio Savastano, Domenico Vespa, Daniela Danieli, Alessandra Costantini, Davide Dal Borgo, Stefano Trupiani, Leonardo Giarraputo.Epidermal cyst of the ischiorectal fossa [Internet]. Italy: Eurorad;2015. Available from: https://www.eurorad.org/case/13168. doi:10.1594/EUROAD/CASE.13168.
- Maruyama T, Ueda Y, Suzuki T, Maeda N, Yoshimoto T, Kondoh N, Nojima M, Takiuchi H, Mori Y, Shima H, Kubota A. [Epidermoid cyst of perineo-scrotal region: report of a case]. Hinyokika Kiyo. 2004 Dec;50(12):885-7. Japanese. PMID: 15682864.
- V.H B, Raja B, Rao N. Giant Epidermoid Inclusion Cyst in the Ischiorectal Fossa: A Case Report.J Clin of Diagn Res.2012; 6(1):103-105. doi:org/10.7860/JCDR/2012/.1864.
- Houdek MT, Warneke JA, Pollard CM, Lindgren EA, Taljanovic MS. Giant epidermal cyst of the gluteal region. Radiol Case Rep. 2015 Nov 6;5(4):476. doi: 10.2484/rcr.v5i4.476. PMID: 27307882; PMCID: PMC4901019. doi: 10.2484/rcr.v5i4.476.
- Ziadi S, Trimeche M, Hammedi F, Sriha B, Jomaa W, Mokni M, Korbi S. Squamous cell carcinoma arising from an epidermal inclusion cyst: A case report. N Am J Med Sci. 2010 Jan;2(1):46-7. PMID: 22624113; PMCID: PMC3354388.