Clinical Outcomes of Double Fascicular Nerve Transfer for Restoring Elbow Flexion in Brachial Plexus Injuries

Article
Introduction
Brachial plexus injuries, though infrequent, exert a profound impact, afflicting only 1% of polytrauma patients [1]. These injuries culminate in compromised motor function and sensation within the affected upper extremity. Predominantly affecting young males, they constitute up to 90% of reported cases [2]. The repercussions of traumatic brachial plexus injuries are far-reaching, inflicting substantial physical disability, psychological distress, and economic hardships on the youthful population. Motor vehicle accidents account for nearly 70% of these cases [3].
Brachial plexus injuries can be classified into upper trunk, lower trunk, isolated roots and trunks, and pan-brachial plexus injuries. Patients with upper arm-type brachial plexus injuries (specifically, involving C5-C6 and C5-C6-C7) demonstrate deficits in shoulder elevation, abduction, external rotation, and elbow flexion functions. Additionally, those with a C7 root injury may experience additional impairments in elbow, wrist, and hand extension functions. The evolution of reconstructive techniques now offers viable solutions, encompassing nerve repair, nerve grafting, nerve transfer, muscle/tendon transfer, and free-functioning muscle transfer, thereby presenting avenues for restoring functionality in upper arm brachial plexus injuries.
Crucial considerations in the realm of surgical management entail a profound understanding of injury patterns, strategic timing of surgical intervention, prioritization of functional recovery, and adept management of patient expectations. Initially, a conservative approach is adopted for all patients unless root avulsion or distal brachial plexus disruption has been confirmed. Patients with an intact brachial plexus undergo a three-month period of observation to monitor signs of regeneration and muscle reinnervation. Following this period, a re-evaluation, complemented by repeat EMG studies, is conducted. In cases where spontaneous recovery is absent, surgery is advocated at the three-month post-injury juncture [4].
A plethora of options exist for restoring elbow flexion, with the optimal approach contingent upon the availability of donor motor nerves. Pioneered by Oberlin et al. in 1994, the transfer of a single ulnar nerve fascicle to the biceps branch of the musculocutaneous nerve emerged as an early technique for restoring elbow flexion. Building upon this foundation, Mackinnon et al. in 2003 advocated for the reinnervation of both the biceps and brachialis muscles, thereby augmenting the potential for robust elbow flexion recovery [5, 6]. The primary aim of this study is to assess the clinical outcome of elbow function subsequent to Modified double fascicular Oberlin transfer, a procedure involving the transfer of ulnar and median nerve fascicles to the musculocutaneous nerve. This study focuses on patients with upper brachial plexus injuries predominantly involving the C5-C6 nerve root.
Methods
A retrospective observational study was conducted on patients who underwent Modified Oberlin transfer for upper brachial plexus injuries at Army Hospital Colombo 05, Sri Lanka, from January 2019 to September 2023. Five consecutive patients who underwent Oberlin transfer at Army Hospital Narahenpita were selected for the study. Electrophysiological studies and MRI of the thoracic outlet were routinely performed to identify root avulsions and establish whether the lesions were pre-ganglionic or post-ganglionic. All patients underwent the Oberlin procedure by a single surgeon approximately 4 months from the date of injury. Patients were placed in a supine position with the abducted and externally rotated arm. An incision was made over the medial aspect of the arm, and the deep fascia was divided. The muscular cutaneous nerve, median nerve, and ulnar nerve were identified. The motor branch of the muscular cutaneous nerve to the biceps and brachialis was identified and divided. A motor branch of the ulnar nerve was identified using a nerve stimulator, and a nerve fascicle was divided by intraneural neurolysis. The biceps was re-innervated with the ulnar nerve fascicle using 8-0 proline, and the median nerve fascicle was separated by intraneural neurolysis and reinnervated to the brachialis motor branch using 8-0 proline. Direct coaptation of the nerve fascicles was performed without the need for nerve grafts, and no nerve glue was applied. The deep fascia was sutured with 5-0 monocryl, and the skin was closed with 5-0 monocryl. A broad arm sling was used postoperatively, and patients were discharged within 72 hours of the procedure. They were advised to perform both active and passive wrist and finger movements starting from post-op day 1, and elbow function was evaluated during weekly clinic visits. Electrical nerve stimulation was initiated at 3 weeks post-op, and physiotherapy was arranged. Elbow flexion power was assessed using the Medical Research Council (MRC) scale 6 and 8 months postoperatively.
Results
The study encompassed five patients, comprising four males aged 22, 35, 32, and 28, and one female aged 65. Notably, all male patients had sustained injuries in road traffic accidents, whereas the female patient’s brachial plexus injury was a consequence of the excision of a schwannoma in the left posterior triangle. All patients presented with predominant upper brachial plexus injuries, exhibiting a pre-surgical biceps power rating of 0. Among these, three patients had injuries on the right side, while the remaining two sustained injuries on the left side. At the 6-month post-surgery, all patients demonstrated functional elbow flexion power surpassing a score of 3. Subsequently, the median elbow flexion power at 8 months post-surgery was 4 (q1=3, q3=4) (Figure 1). Kruskal-Wallis test with post-hoc Dunn’s multiple comparisons indicated a statistically significant improvement of elbow flexion power postoperatively (H(2)=11.08, p=.001) (Figure 1). Furthermore, none of the patients exhibited any sensory or motor deficits within the ulnar or median territories subsequent to the surgical intervention.
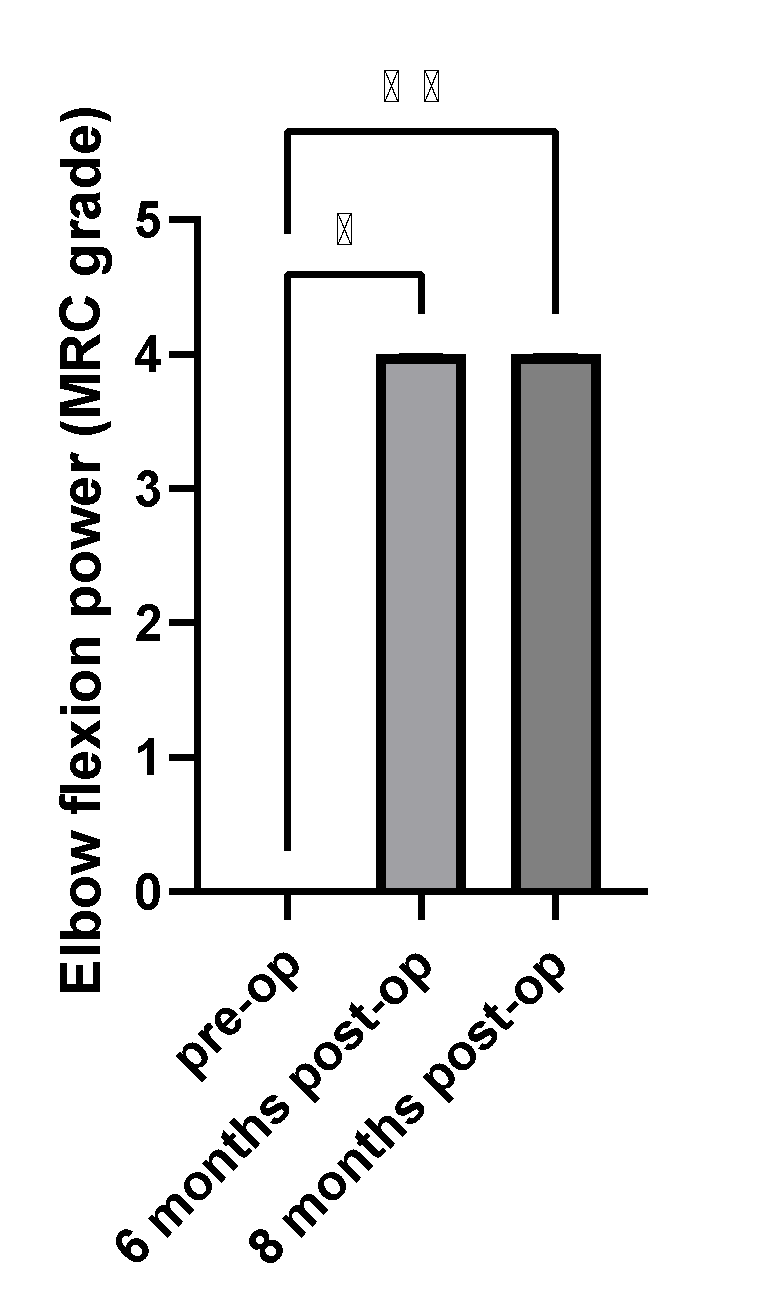
Figure 1. Functional outcomes of double fascicular nerve transfer for restoring elbow flexion in brachial plexus injuries. Median elbow flexion power tested preoperatively, 6 months after the surgery and 8 months after the surgery. Error bars are interquartile range. *p<.05, *p<.01
Discussion
The current study underscores the effectiveness of Modified double fascicular Oberlin transfer in addressing upper brachial plexus injuries predominantly involving the C5-C6 nerve root. Our results demonstrate an excellent improvement of elbow flexion power within 6 months postoperatively. Despite these promising findings, it is crucial to acknowledge certain limitations. The study’s sample size remains modest, warranting further investigations with larger cohorts. Additionally, while the study assesses the immediate postoperative outcomes, a longitudinal evaluation would offer valuable insights into the durability of the functional improvements.
In conclusion, the transfer of expendable motor fascicles from the ulnar and median nerves proves to be a highly effective method for reinnervating both the biceps and brachialis muscles, culminating in robust elbow flexion. Notably, this approach offers an additional biomechanical advantage by reinvigorating the brachialis muscle, a pivotal contributor to elbow flexion. The synergistic activation of these key muscles underscores the exceptional functional restoration achieved through this surgical intervention. This technique not only optimizes motor performance but also holds significant promise for enhancing the overall quality of life for individuals with upper brachial plexus injuries.
Conflicts of interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding
This research received no specific grants from any funding agency in the public, commercial or not-for-profit sector.
Acknowledgements
None
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author(s).
References
-
P.D. Choi et al. Quality of life and functional outcome following brachial plexus injury. J. Hand. Surg. Am. (1997)
-
G.A. Brunelli et al. Modified steindler procedure for elbow flexion restoration. J. Hand. Surg. Am. (1995)
-
1. Narakas AO, Hentz VR. Neurotization in brachial plexus injuries. Indication and results. Clin Orthop Relat Res.1988;(237):43-56
-
M.D. Vekris et al. Restoration of elbow function in severe brachial plexus paralysis via muscle transfers Injury. (2008)
-
Oberlin C, Beal D, Leechavengvongs S, Salon A, Dauge MC, Sarcy JJ. Nerve transfer to biceps muscle using a part of ulnar nerve for C5-C6 avulsion of the brachial plexus: anatomical study and report of four cases. J Hand Surg Am. 1994;19(2):232-237.
-
Mackinnon SE, Novak CB, Myckatyn TM, Tung TH. Results of reinnervation of the biceps and brachialis muscles with a double fascicular transfer for elbow flexion. J Hand Surg Am. 2005;30(5):978-985