Novel concept for non-healing ischial decubitus ulcers with histological analysis of two cases

Abstract
Decubitus ulcers are often related to sustained pressure on soft tissues trapped between two hard surfaces. Currently, this concept has been challenged due to better understanding of the differences in pathophysiology of ulcer progression. This article will focus on the anatomy of Ischial region, physiological adaptation and pathophysiology of the pressure ulcers. Finally, describes possible mechanisms of poor-healing of those ulcers using two case vignettes.
Article
Introduction
Ischial region anatomy
Ischial tuberosity has evolved with humans to play a significant role in posture, stability and bipedal mobility. It is a central structure that act as a fulcrum for muscles and ligaments. While the medial segment provides direct support to the axial load of the body, rest of the surface provides attachment for Semitendinosus long head of biceps femoris tendon complex. Semi membranous is attached towards the lateral margin. The medial lip is covered with the sacro-tuberous ligament [1].
This ischial complex is covered by gluteus Maximus on standing position. The same muscle moves away with the seated position in majority of male and female bodies. Bulk tissue thickness varies from few millimetres to few centimetres at the apex of the tuberosity. This makes the soft tissue under the tuberosity to be particularly vulnerable for ischaemia. Ischial bursa provides the gliding surface to the tuberosity [1].
Ischial bursa is a synovial type of sack that is similar to the lining of a joint. This provides a gliding surface for the buttock skin: i.e. to glide over the tuberosity. Magnetic resonance imaging shows that although superficial surface of the bursa is not firmly adhered, the deep surface of the synovium is firmly adherent to the bone [1].
Pathophysiology of pressure injury to skin
Aetiology of pressure injury is a combination of four mechanical and circulatory factors (2)
- tissue deformation leading to direct cellular injury
- Occluded capillaries causing ischaemia
- Tissue injury due to reperfusion
- Lymphatic dysfunction causing accumulation of toxins.
These mechanisms are mostly applicable to deeper tissues. Superficial lesions are mostly related to friction damage to skin. In contrast to earlier understanding of grade 1 pressure ulcers even with the intact epidermis dermal capillary, smaller veins may show stasis, extraversation and fat necrosis. Deeper structures are also vulnerable for pressure and shear induced smaller vessel rupture and blockage. These were evident on several histological studies done on pressure ulcers [4]. However, the earlier animal model studies revealed the friction alone will not cause ischeamia[3]. These elaborated electron and light microscopic studies describe intra-cellular changes and typical pressure induced ishaemia to tissue architecture. This has been postulated to be a precursor to invasive infections that further complicates the injury. During the latter part of the ulcer development healing starts at the periphery. The pressure ulcers show several different pathways in the clinical course. This is especially true for patients who has improved nursing care and offloading of the pressure on the area. Converse is true for patients with poor nutrition, sepsis, or local infection. We believe the clinical course of the wound is related to site since local complications of each type varies.
The commonest presentation of ischial pressure ulcer in our series is the chronic discharging small wound with a fibrotic rim. The non healing nature of these cases was analysed using ulcer histology.
Case details
We selected 2 patient who underwent V-Y advancement flap repair for ischia pressure ulcers. Both were male patients aged 58 and 47 years, with paraplegia due to previous vertebral fractures. Apart from flap reconstruction, we performed En block excision of ischial ulcer up to the periosteum of the ischium. In both patients’ histology showed Evidence of oedematous granulation tissue near the keratinized squamous epithelium (Which denotes the adjacent area of the skin margin) and polypoid contours resembling synovial tissue (Figure 1 and figure 2). There were no evidence of invasive malignancy or granuloma formation.
Discussion
The ischial ulcer histology indicates thick fibrosis and synovial membrane covering the ulcer. The fibrosis is explained by the wound contraction lead by myofibroblast theory. Synovial membrane lining the bursa has proliferated to line the cavity[4]. This could be a response to counteract the pressure and the friction on ulcer cavity wall. There is evidence that this is related to several trigger mechanisms; pressure, increased local temperature, prolong inflammation, that causes genetic alterations. These altered genetic expressions can lead to a sustained local response of proliferative tendencies of the bursa synovium. These exact markers are not yet identified. Reasons for non-closure of this unnamed pathological connection between a synovium lined cavity and skin could be a combination of pressure, contact inhibition of skin, wound edge hyper keratosis or the synovial fluid discharge.
Although pressure effect on the pressure ulcer healing has been studied the extent of contact inhibition influence on non-closure is poorly understood in ischial ulcers. Wound edge hyper keratosis could be similar to callus formation in neuropathic foot. Discharging wounds are known to keep cavity connections open. The synovial like fluid that is produced by the ulcer could very well be an additional factor for non-healing nature of these ischial pressure ulcers. The amount of granulation tissue is minimal compared with any other common ulcer. This may be a distinct feature of these open bursa type lesions on the ischial tuberosities. The normal superficial bursa synovium produces very small quantities of hyaluronan. There are no reports of contents of the ischial pressure ulcer discharge. The proliferation of these ulcer synovial cells is different to rheumatoid arthritis since the invasive features are not seen on histology[5]. The finer cellular features and the matrix character has not been compared with rheumatoid tissue up to now.
Conclusion
Ischial pressure ulcer can behave similar to an open bursa. Once stable they can persist for long durations. Proliferative synovium and skin keratosis remain key pathologies preventing resolution in stable ischial pressure ulcers. The term ulcer may not be the most suitable term since it shows minimal granulation on the base of the ulcer. Hence, we propose the term ischial syconia.
Declarations
none
ORCID
Gayan Ekanayake https://orcid.org/0000-0001-8420-7073
Oshan Basnayake https://orcid.org/0000-0002-1239-7506
Ethics approval and consent to participate:
Not applicable
Consent for publication
Informed written consent for publication and accompanying images was obtained from the patients prior to collecting information.
Availability of data and material:
All data generated or analyzed during this study are included in this published article
Competing interests:
The authors declare that they have no competing interests.
Funding:
The authors received no financial support for the research, authorship, and/or
publication of this article.
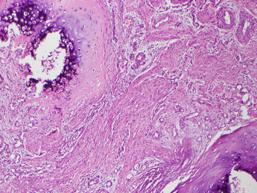
Figure 1 Patient A Histology , The section shows synovial tissue and a foci of new bone formation
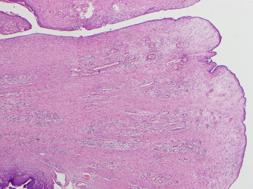
Figure 2 Patient A, The slide shows a typical fleshy synovial proliferation with no epithelium
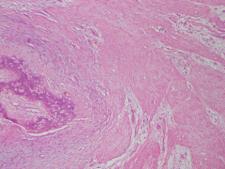
Figure 3 Patient B, The section shows a cartilage element within the synovial stroma.
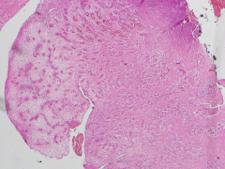
Figure 4 Patient B, Shows a ploypoidal segment of the fleshy synovial folds seen inside the ishial pressure syconia

Figure 5 Typical appearance of an ischial syconium. Note the smaller fibrotic opening and fleshy inside.

Figure 6 V to Y flap design to advance once the en bloc excision is done.
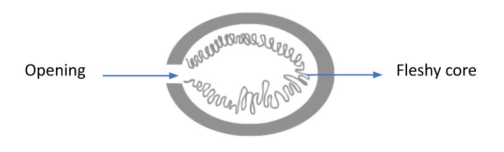
Figure 7: Cross-section of a Ficus fruit
References
- Ripani M, Continenza MA, Cacchio A, Barile A. The ischiatic region: normal and MRI anatomy. Journal of sports medicine and physical fitness. 2006 Sep 1;46(3):468.
- Bain M, Hara J, Carter MJ. The Pathophysiology of Skin Failure vs. Pressure Injury: Conditions That Cause Integument Destruction and Their Associated Implications. Wounds: a compendium of clinical research and practice. 2020 Nov 1;32(11):319-27.
- Kesarwani A, Nagpal PS, Chhabra HS. Experimental animal modelling for pressure injury: A systematic review. Journal of Clinical Orthopaedics and Trauma. 2021 Jun 1;17:273-9.
- Fleming LT, Leung PH. Effects of friction and pressure on skin in relation to pressure ulcer formation. InInnovations and Emerging Technologies in Wound Care 2020 Jan 1 (pp. 281-291). Academic Press.
- Hirohata S, Sakakibara J. Synovial histopathology in early rheumatoid arthritis. Arthritis Research & Therapy. 1999 Nov;1:1-24.