Thenar motor branch: keeping variations in mind
Abstract
Carpal tunnel syndrome is the commonest type of entrapment neuropathy in the upper limb. Increased pressure within the carpal tunnel, >32 mmHg, leads to vascular ischaemia of the median nerve causing primarily nocturnal pain and paraesthesia involving the radial 31/2 digits, worsening with wrist flexion, and increased difficulty in fine motor tasks.
Variations in the course of branches of the median nerve particularly its thenar motor branch (TMB) have been extensively studied. Surgical decompression of the carpal tunnel is a commonly performed surgery and awareness of such variations is critical to prevent iatrogenic injury.
Here we present a case of a 35 year who underwent surgical decompression of the carpal tunnel under loupe magnification in a plastic surgery unit. Careful dissection of the hypertrophied muscle over the transverse carpal ligament (TCL) revealed a nerve emerging through the ligament. An ulnar approach employed to divide the TCL and decompress the median nerve confirmed it as the transligamentous variant of the TMB arising from the anterior surface of the median nerve.
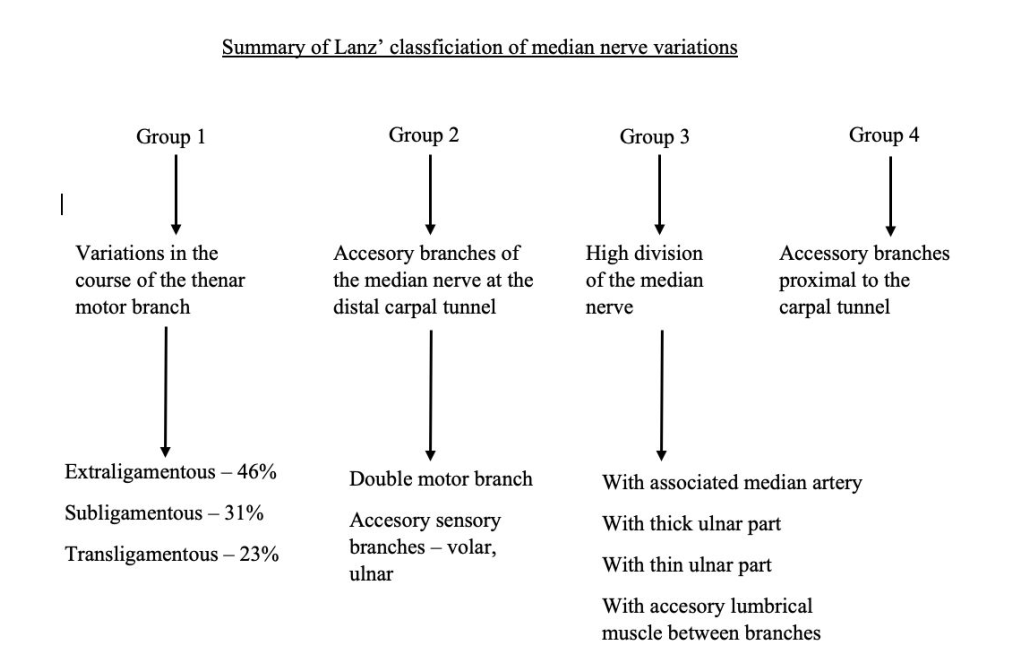
Poisel’s original classification divided the TMB into extraligmentous, subligamentous and transligamentous variants. Lanz further expanded on this classification. The rare transligamentous course, seen in 1 in 10 people is at highest risk of iatrogenic injury in hand and wrist surgery. Nicknamed the “million-dollar nerve”, damage to the TMB is a surgeon’s nightmare owing to the high legal costs faced with litigation.
Awareness of and clinical suspicion of such variations along with meticulous surgical technique, with layer by layer dissection, is mandatory to prevent iatrogenic injury
Article
CLINICAL QUESTION/LEVEL OF EVIDENCE:
Therapeutic, IV
Introduction
Carpal tunnel syndrome is the commonest type of entrapment neuropathy in the upper limb. Increased pressure within the carpal tunnel, >32 mmHg, leads to vascular ischaemia of the median nerve resulting in a range of symptoms that include nocturnal pain and paraesthesia involving the radial 31/2 digits, particularly worsening with wrist flexion, and increased difficulty in fine motor tasks (1).
Increased pressure within this compartment could be either due to an increase in volume of its contents, or decreased size of the tunnel itself. Causes for increased volume of its components could be primary, due to anatomical abnormalities, or secondary to systemic conditions such as diabetes, rheumatoid arthritis, hypothyroidism, acromegaly and pregnancy (1).
Anatomical variations within the carpal tunnel have been described in relation to nerves, vessels, muscles and tendons (3). Variations in the course of branches of the median nerve particularly its thenar motor branch have been extensively studied (4). Surgical decompression of the carpal tunnel is a commonly performed surgery and awareness of such variations is critical to prevent iatrogenic injury (1).
Here we describe an encounter with a transligamentous variant of the thenar motor branch encountered during carpal tunnel decompression.
Case Report
A 35-year-old previously well Sri Lankan female presented to the plastic surgical clinic with pain and tingling along the radial half of the right hand for 2 months’ duration. The pain was worse at night and with activities that involved flexion of the wrist, such as driving and cooking. There was recent onset clumsiness with dropping objects due to difficulty in forming a tight grip. There was no associated neck pain or pain radiating along the arms. She was right handed and a doctor by profession.
On examination, she had paresthesia over the radial half of the fingers without involvement of the skin over the thenar eminence. There was no muscle wasting but mild weakness of the abductor pollicis brevis muscle. Tinel’s and Phalen’s signs were positive. A clinical diagnosis of carpal tunnel syndrome was made. Nerve conduction studies were confirmatory.
Open carpal tunnel decompression was performed using loupe magnification. Upon dissecting through the palmar aponeurosis, hypertrophied muscle was seen arising from the transverse carpal ligament (TCL). Following careful dissection of the muscle, a nerve was seen piercing the TCL and supplying the thenar muscles. Careful division of the TCL depicted its origin from the upper aspect of the median nerve within the carpal tunnel, confirming this as the transligamentous variation of the thenar motor branch of the median nerve.
Following decompression, she made an uneventful recovery and significant improvement in nocturnal paraesthesia at 1 month.

Fig 1: The thenar motor branch of the median nerve seen arising from the anterior aspect of the median nerve within the carpal tunnel and piercing the transverse carpal ligament.
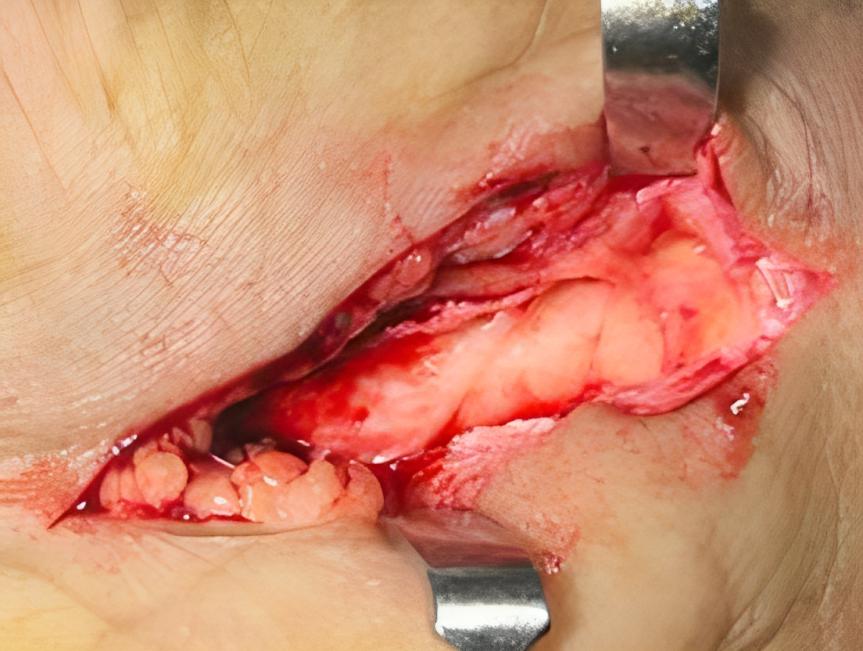
Fig 2: A closer look at the transligamentous TMB arising from te anterior aspect of the median nerve within the carpal tunnel and piercing the transverse carpal ligament
Discussion
Carpal tunnel syndrome is the commonest type of entrapment neuropathy. Increased pressure within the carpal tunnel in excess of 32mmHg leads to ischaemia and compression of the median nerve within the carpal tunnel (1). The median nerve, a mixed nerve, traverses the wrist through the carpal tunnel deep to the transverse carpal ligament (TCL) and divides into medial and lateral branches upon exiting the tunnel at the distal border of the TCL. The recurrent thenar motor branch arises from the lateral branch, before giving rise to proper palmar digital nerves. The thenar motor branch (TMB), exclusively supplies the abductor pollicis brevis muscle, and with the ulnar nerve co-innervates the flexor pollicis brevis and opponens pollicis (2,4). Hence, ischemia and compression of the nerve within the carpal tunnel leads to nocturnal paresthesia over the radial 31/2 fingers and difficulty in fine motor skills (1).
Numerous anatomical variations have been described in literature in relation to the nerves, vessels, muscles and tendons that are components of the carpal tunnel (3). Particular importance has been placed on variations in the course and branches of the median nerve, of which the TMB is of paramount importance (4). Yet only the typical extraligamentous type is described in most anatomical text books. Nicknamed the “million-dollar nerve” due to high legal costs faced by surgeons due to litigation caused by accidental injury the nerve during hand and wrist surgery, intimate knowledge of the variations to the TMB is essential armor to a surgeon (6,7).
The Poisel classification divided the TMB into 3 groups based on its branching pattern; the commonest extraligamentous (Type I), subligamentous (type II) and transligamentous (type III) (5). In the extraligamentous type, the TMB arises from the median nerve at the distal end of the TCL, and hooks over its free border before travelling in a retrograde manner to reach the thenar musculature. In the subligamentous type, the TMB arises from the median nerve within the carpal tunnel deep to the TCL, and then enters the thenar in a similar fashion to type 1. In the rarer trans-ligamentous type, the TMB arises within the carpal tunnel, but pierces the TCL to then reach the overlying thenar muscle (5,9).
Lanz expanded Poisel’s original classification system, to include variations of the median nerve in the carpal tunnel (8). He described four groups of variations: variations in the course of the single TMB according to Poisel (type 1), accessory branches of the median nerve at the distal carpal tunnel (type 2), high division of the median nerve (type 3), which Lanz reported to be associated with the presence of a persistent median artery (PMA) running with the bifid median nerve, and accessory branches of the median nerve proximal to the carpal tunnel (type 4) (4,8).
Multiple studies have been conducted to assess anatomical variations of the TMB with results varying depending on the classification system used. A meta-analysis by Henry et al found the extra-ligamentous course of the TMB to be the commonest with a pooled prevalence rate of 75.2%. The sub-ligamentous group was seen more commonly in those undergoing intraoperative procedures that in cadaveric group (24.6% vs 13.5%) which indicate that this variation may be associated with a higher risk of CTS (3,4,9).
The prevalence of the transligamentous course varied from 0 to 80% amongst studies with a pooled prevalence rate of 11.3%. Variations in interpretations of nerves that arise outside the TCL but that pierce the oblique fascia of TCL as in fact trans-ligamentous may be a cause for high prevalence in some studies (4). Lanz suggested that the trans-ligamentous course was associated with a higher risk of CTS. The pooled prevalence for ulnar side of branching of the TMB was 2.1% (95% CI: 0.9%- 3.6%), while the pooled prevalence for radial/anteroradial side of branching was 97.9%. The trans-ligamentous variation is at highest risk of iatrogenic injury during CTD followed by the sub-ligamentous counterpart (4,8).
Adding to this complexity, the presence of hypertrophied muscle mixed in with TCL seen in 18.2% of patients should serve as a warning sign to underlying anatomical variations of the TMB, as a transligamentous course was seen in 23.4% of those with hypertrophied muscle as compared to 1.7% of without it. Therefore, an ulnar side approach, with layer by layer dissection of the carpal tunnel is recommended to prevent iatrogenic injury (4,7).
The above case describes an encounter with the transligamentous variation of the TMB seen in roughly 1 in 10 patients undergoing carpal tunnel decompression. It arose from the anterior surface of the nerve. Recognition was hampered by the presence of hypertrophied thenar muscles interspersed with the TCL encountered during carpal tunnel release. Layer by layer dissection under loupe magnification and an ulnar approach aided its timely recognition.
Conclusion
An array of anatomical variations has been described in the carpal tunnel most notably for the TMB of the median nerve. Hypertrophied thenar muscles over the TCL should raise suspicion over the presence of a variant. An ulnar approach to division of the TCL is recommended to minimize the risk of iatrogenic injury.
Consent:
Informed written consent was obtained from the patient for publication inclusive of images.
Ethical Approval
Not applicable
Author information
Deshan Gomez1. https://orcid.org/0000-0001-7448-1861
Gayan Ekanayake2 https://orcid.org/0000-0001-8420-7073
Competing interest:
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
None
Open access
AJPRS is an open access journal. This work is licensed under CC BY-NC 4.0
How to site this article
Copyright © 2024 by Sri Lanka Association of Plastic Reconstructive and Aesthetic Surgeons
References
-
Cha J, York B, Tawfik J. The recurrent motor branch of the median nerve. Eplasty. 2013 Dec 24;13:ic63. PMID: 24498458; PMCID: PMC3881213.
-
Chammas, M., Boretto, J., Burmann, L., Ramos R.M., Santos Neto, F.C. dos., & Silva, J.B., (2014). Carpal tunnel syndrome – Part I (anatomy, physiology, aetiology and diagnosis). Revista Brasiliera De Ortopedia 49(5), 429-436. http://doi.org/10.1016/j.rboe.2014.08.001
-
Mitchell R, Chesney A, Seal S, Mcknight L, Thoma A. Anatomical variations of the carpal tunnel structures. Canadian Journal of Plastic Surgery. 2009;17(3):3-7. doi:10.1177/229255030901700302
-
Henry BM, Zwinczewska H, Roy J, Vikse J, Ramakrishnan PK, Walocha JA, et al. (2015) The Prevalence of Anatomical Variations of the Median Nerve in the Carpal Tunnel: A Systematic Review and Meta-Analysis. PLoS ONE 10(8): e0136477. https://doi.org/10.1371/journal.pone.0136477
-
Poisel S. Ursprung und Verlauf des R. muscularis des Nervus digitalis palmaris communis I (N. medianus), Chir Praxis 18: 471–474, 1974.
-
Krishnan P, Mishra R, Jena M, Das A. Trans-ligamentous thenar branch of the median nerve: the million-dollar nerve. Neurol India 2013;61(3):311–2. pmid:23860158 PubMed/NCBI Transligamentous+thenar+branch+of+the+median+nerve%3A+the+million+dollar+nerve+Krishnan+2013" target="Go to article in Google Scholar">Google Scholar
-
Al-Qattan MM. Variations in the course of the thenar motor branch of the median nerve and their relationship to the hypertrophic muscle overlying the transverse carpal ligament. J Hand Surg Am 2010;35(11):1820–4. pmid:20934817 PubMed/NCBI Google Scholar
-
Lanz U. Anatomical variations of the median nerve in the carpal tunnel. J Hand Surg Am 1977;2(1):44–53. pmid:839054 PubMed/NCBI Google Scholar
-
Scott H. Kozin, The anatomy of the recurrent branch of the median nerve, The Journal of Hand Surgery, Volume 23, Issue 5, 1998, Pages 852-858, ISSN 0363-5023, https://doi.org/10.1016/S0363-5023(98)80162-7.